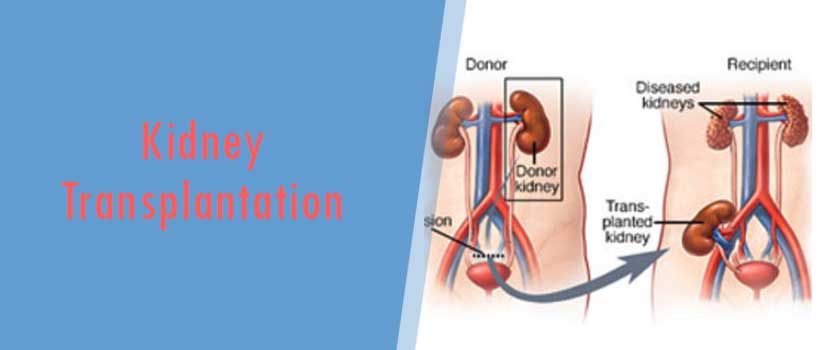
Kidney Transplantation
INTRODUCTION
Kidney transplantation in the last 65 years has enjoyed remarkable progress with the development of novel immunosuppressants, antirejection therapy and various surgical procedures. This has resulted into huge success in the field of renal transplantation.
HISTORY
The first clinical cadaver renal transplant was performed in 1933 by the Ukrainian surgeon Voronoy, with unsuccessful results secondary to the immunologic barrier. In the 1950’s these obstacles were circumvented by performing the procedure between identical twins. The era of modern renal transplantation began with the introduction of azathioprine to suppress the human immune system. With the demonstration of the synergistic effect of glucocorticoids, renal transplantation was established as a viable option for the treatment of ESRD. This was followed soon by the development of polyclonal antilymphocyte agents such as ALG which contributed significantly to the treatment of acute rejection (AR). Immunosuppression remained relatively constant for the next 15 years until the 80’s, and the introduction of cyclosporine A (CyA). At that time, it was the most specific immunosuppressive agent known. It resulted in significant improval in graft and patient survival rates, not only after kidney transplantation, but after all organ transplants, thus allowing for a dramatic increase in extrarenal transplants.
INDICATIONS AND PREOPERATIVE EVALUATION
For the majority of people with ESRD, transplantation results in superior survival, improved quality of life and lower costs as compared with chronic dialysis. There are very few absolute contraindications and so most patients with ESRD should be considered as potential candidates. The subsequent lifelong immunosuppression is associated with considerable morbidity. Therefore, evaluation of a potential recipient must focus on identifying risk factors that could be minimized or may even contraindicate a transplant.
The preoperative evaluation can be divided into four phases: medical, surgical, immunologic, and psychosocial. The medical evaluation begins with a complete history and physical examination. Any history of congestive heart failure, angina, myocardial infarction or stroke should be elicited. Patients with symptoms suggestive of cardiovascular disease or significant risk factors (e.g. diabetes, age over 50, previous MI) should undergo further cardiac evaluation. Echocardiography should be performed if patients have evidence of valvular disease or a history of congestive heart failure, to determine left ventricular ejection fraction. Any problems identified should be treated appropriately (medically or surgically); patients whose cardiovascular problems are too severe should not undergo transplantation. Patients with suspected cerebrovascular disease should undergo evaluation with carotid duplex Doppler studies.
Untreated malignancy and active infection are absolute contraindications to transplantation because of the requisite lifelong immunosuppression. Following curative treatment of malignancy, an interval of 2 to 5 years is recommended prior to transplantation. This recommendation is influenced by the type of malignancy, with longer observation periods for neoplasms such as melanoma or breast cancer and shorter periods for carcinoma in situ or low grade malignancies such as basal cell carcinoma of the skin. Chronic infections such as osteomyelitis or endocarditis must be fully treated. Other areas of the medical evaluation should concentrate on gastrointestinal problems such as peptic ulcer disease, symptomatic cholelithiasis, and hepatitis. Patients with ulcers should receive appropriate treatment followed by endoscopic evaluation to document resolution. Cholelithiasis should be treated by cholecystectomy prior to the transplant. Patients who are hepatitis C positive, but have no evidence of active hepatic inflammation, are acceptable transplant candidates. Whether patients with hepatitis B should be transplanted is controversial. There is an increased risk in these patients of developing chronic active hepatitis and cirrhosis after receiving immunosuppression, but many have excellent long-term survival rates and improved quality of life compared with those on chronic dialysis. Therefore, many centers feel that chronic hepatitis B infection, in the absence of cirrhosis or active viral replication, is not a contraindication to transplantation.
The surgical evaluation should concentrate on identifying vascular or urologic abnormalities that may affect transplantation. Evidence of vascular disease that is revealed by the history (claudication or rest pain) or the physical examination (diminished or absent pulse, bruit) should be evaluated further by Doppler studies or angiography. Urologic evaluation should rule out chronic infection in the native kidney, which may require nephrectomy pretransplant. Other indications for nephrectomy include huge polycystic kidneys, significant reflux, or uncontrollable renal vascular hypertension. Children especially require a complete GU tract examination to evaluate reflux and bladder outlet obstruction.
An assessment of the patient’s immunologic status involves determining blood type, tissue type (HLA A,B,DR antigens), and presence of any cytotoxic antibodies against HLA antigens (because of prior transplants, blood transfusions, or pregnancies).
A psychosocial evaluation is necessary to ensure that patients understand the nature of the transplant procedure, with its attendant risk. They must be capable of following the medical regimen following the transplant. Patients who have not been compliant with their medical regimen in the past must demonstrate a willingness and capability to do so, before they undergo the transplant.
Finally, it is important to remember that patients may be on the cadaver organ waiting list for prolonged periods. Regular reevaluation is necessary to search for any progression of underlying or new disease that may require attention or may contraindicate transplantation.
DONOR EVALUATION
Living donors are preferred over cadaver donors. Recipients of living donor organs enjoy improved long-term success, avoid a prolonged wait and are able to plan the timing of their transplant in advance. Moreover, they have a significantly decreased incidence of ATN, increased potential for HLA matching and the opportunity to initiate and optimize immunosuppression therapy preoperatively. All of these advantages contribute to a lower incidence of early acute rejection and to improved graft and patient survival rates. While there is significant benefit for the recipient, there is no physical benefit for the living donor, only potential for harm. Therefore, it is paramount that the risks of donation are acceptably low, that the donor is fully aware of the potential risks, and has freely given informed consent. Laboratory evaluation of the donor should include basic blood tests (e.g. CBC, electrolytes, glucose, viral serology), assessment of renal function (serum creatinine, creatinine clearance, urinalysis) and an anatomic evaluation of the kidneys (IVP, angiogram). With appropriate preoperative screening, the risk of a lethal complication as a result of donation is estimated to be less than 0.05%. The incidence of postoperative complications was roughly 8% in one large series; most of these were relatively minor. Living unrelated donors are being used with increasing frequency, with excellent results, comparable to living related (non-HLA identical) donors.
In the absence of living donors, transplant candidates are placed on the cadaver organ waiting list. Determining the appropriateness of a given cadaver donor depends on that donor’s medical history (e.g. age, diabetes, increased blood pressure, any known kidney abnormality or previous malignancy) and pre-donation renal function. The serum creatinine is the most useful measurement of renal function. It is important to determine the admission creatinine, its trend over the duration of hospitalization, as well as the reversibility of any elevation with appropriate measures such as hydration. With marginal renal donors (e.g. those with hypertension or diabetes, or those over age 65 but with normal serum creatinine), the kidneys should be biopsied at the time of procurement. As long as less than 10% of examined glomeruli are sclerotic, long-term success rates are good.
Medical Requirements
Compatible blood group; similar to blood donation.
Recipient workup; these tests are done to ascertain the fitness of the patient for the transplant and care required after transplant Fitness to undergo major surgery will include an age appropriate cardiac workup like ECG/ ECHO/ stress test / and coronary angiogram in select cases. A detailed liver work in also required in select cases.
Donor workup; these are test of the donor so that she or he can go through surgery without problem and the kidney given to patient is of good quality All routine test like CBC/ renal profile/ liver function tests / cardiac workup for fitness of surgery/ viral markers- HIV/ HCV/HbsAg. USG abdomen / renal scan / CT-IVP and CT angiogram for determining the renal function of both kidneys
Immunological workup. This help us decide about the possibility of rejection etc. Lymphocyte cross match HLA; this test is to be done in India in presence of the nephrologist.

Comments